Worldwide, 47.5 million people are living with dementia. This is expected to increase to 75.6 million by 2030 and more than triple by 2050, according to the World Health Organization (WHO).1
Dementia is not a disease in itself but rather is a term used to describe a number of different brain illnesses that may affect your memory, thinking, behavior and ability to perform everyday activities. The most common type of dementia is Alzheimer’s disease, which accounts for 60 percent to 80 percent of cases.2
Many people associate dementia with memory loss — and this is a red flag — however, not all memory problems are due to Alzheimer’s (and some causes of dementia-like symptoms, including memory loss, can be reversed, such as those related to thyroid problems and vitamin deficiencies).3
If you’ve noticed yourself or a loved one becoming increasingly forgetful or experiencing changes in thinking abilities, you should see a health care provider right away.
Oftentimes, however, the first symptoms are so subtle they may be easily missed — and they may manifest as changes in behavior and mood long before memory problems become apparent.
Personality Changes May Be an Early Dementia Sign
Before memory and thinking problems become obvious, people with dementia may display changes in mood and behavior, according to a team of neuropsychiatrists and Alzheimer’s experts, who say the latter symptoms may be among the earliest signs of dementia.
At the 2016 Alzheimer’s Association International Conference (AAIC) in Toronto, the team released a 34-question checklist they believe could eventually be used to diagnosis a new condition called mild behavioral impairment (MBI).
Similar to mild cognitive impairment (MCI), which is defined by a noticeable decline in cognitive abilities that does not yet interfere with most daily functions, MBI describes changes in behavior and mood that may occur prior to MCI and the cognitive changes associated with dementia.
The checklist is intended to identify patients at risk of dementia earlier, as according to team member Dr. Zahinoor Ismail, a neuropsychiatrist at the University of Calgary, among people with MCI, those with mood and behavior changes will progress to full-blown dementia faster.4
Some have expressed concern that the checklist may lead to overdiagnosis or false diagnosis, putting some people through increased medical testing and worry unnecessarily.
In the case of MCI, for instance, not everyone diagnosed will go on to develop Alzheimer’s or other types of dementia. In fact, the Times reported, up to 20 percent of those with MCI later turn out to be cognitively normal.5
Still, others say keeping an eye out for unusual behavioral or personality changes can help people get help, at least symptom relief, faster. Sadly, there is currently no cure for Alzheimer’s disease and, as it progresses, the disease is devastating not only for those diagnosed but also their friends and family.
In order to raise awareness, an Ohio man has been documenting his mother’s battle with Lewy body dementia (LBD), which has symptoms similar to Alzheimer’s. In the video below, he recorded the first time she forgot who he was.6
What Are Some Behavioral or Mood Changes to Watch Out For?
Dementia can manifest itself differently in everyone, which is why the most important changes to watch out for are those that are unusual for your loved one. A person may, for instance, stop doing something they’ve always loved to do, be it cooking a certain dish for your birthday or watching the evening news.
Apathy is another common sign, although some people may display more blatant changes like suddenly becoming sexually promiscuous or developing the habit of snatching food off other people’s plates.7 The Alzheimer’s Association noted:8
“The mood and personalities of people with Alzheimer’s can change. They can become confused, suspicious, depressed, fearful or anxious. They may be easily upset at home, at work, with friends or in places where they are out of their comfort zone.”
In the early stages of the disease, irritability, anxiety or depression may occur. In fact, a study published in the journal Neurology not only found that people who eventually developed dementia were twice as likely to develop depression earlier on in their lives, but they also tended to display mood changes in a consistent pattern.9 Time reported:10
“The symptoms appeared in consistent phases: first, irritability, depression and nighttime behavior changes; followed by anxiety, appetite changes, agitation and apathy. The final phase was elation, motor disturbances, hallucinations, delusions and disinhibition.”
In order for early mood and/or behavioral changes to be considered MBI, the change in behavior must persist for at least six months. Maria C. Carrillo, Ph.D., chief science officer, Alzheimer’s Association, explained in a news release:11
“Alzheimer’s is a deadly brain disease, and while memory loss is a hallmark of the disease, early symptoms such as anxiety, confusion and disorientation are often more common, troubling and obvious to family members.
This proposed new checklist describes and helps identify a new clinical stage in the disease and has the potential to represent a paradigm shift in formal neurodegeneration testing — away from a sole focus on the memory to also encompass behavior.”
Signs of Mild Cognitive Impairment
In some people, MCI may follow the earliest changes in mood and behavior. MCI is a slight decline in cognitive abilities that increases your risk of developing more serious dementia, including Alzheimer’s disease (although it is by no means a guarantee). It’s estimated that up to 20 percent of people aged 65 and older may have MCI.12
Simply misplacing your keys on occasion is not cause for alarm, however forgetting important information that you would have normally recalled, such as appointments, conversations or recent events, may be a sign.
You may also have a harder time making sound decisions, figuring out the sequence of steps needed to complete a task, or judging the time needed to do so.
If you’ve been diagnosed with MCI, be aware that some cases do not progress and may even improve. Regular exercise, proper diet and engaging in mentally and socially stimulating activities may help to boost your brainpower.
Dementia: When to Worry?
It can be difficult to gauge if a loved one is declining mentally. If you have suspicions but aren’t sure, try keeping a notebook to jot down instances that concern you. You may be able to identify a pattern of events that makes the picture clearer.
“Agnes B. Juhasz, nurse, dementia care specialist and author of ‘The Dementia Whisperer: Scenes From the Frontline of Caring,’ suggested making note of anything out of ordinary for that particular person. She wrote in the [U.K.]’s Mirror news:13
‘Naturally, there are a few typical signs and possible changes that are worth watching out for more closely.
These include the level of forgetfulness; acute or permanent confusion about certain things; disorientation in time and place; significant changes in behavior and personality; decreased judgment; changes in speech or writing; and withdrawal from social interactions and activities.
But all these suggested signs ultimately lead us back to the essential, magical question we always have to ask before we can arrive at any further conclusions: ‘Is this abnormal for this individual, or is it part of who they have always been?’ When we notice that something is new and odd, that has never occurred in a person`s life before, as far as we have observed, that is the point when further help may be needed.’”
Early Warning Signs of Alzheimer’s
While absent-minded mistakes, like putting a mug in the wrong cabinet, is not a cause for alarm, feeling confused about day-to-day tasks is.
Losing interest in hobbies, repetitive behaviors (phrases, gestures or questions), mispronouncing words or stuttering can also be signs. And while typical forgetfulness, like forgetting why you were walking into a room, is not typically reason to worry, more profound confusion, like the room itself feeling unfamiliar, may signal a problem.14
The Alzheimer’s Association also compiled differences between symptoms of dementia including Alzheimer’s and typical age-related changes:15
| Signs of Alzheimer’s/dementia | Typical age-related changes |
|---|---|
| Signs of Alzheimer’s/dementia: Poor judgment and decision-making | Typical age-related changes: Making a bad decision once in a while |
| Signs of Alzheimer’s/dementia: Inability to manage a budget | Typical age-related changes: Missing a monthly payment |
| Signs of Alzheimer’s/dementia: Losing track of the date or the season | Typical age-related changes: Forgetting which day it is and remembering it later |
| Signs of Alzheimer’s/dementia: Difficulty having a conversation | Typical age-related changes: Sometimes forgetting which word to use |
| Signs of Alzheimer’s/dementia: Misplacing things and being unable to retrace steps to find them | Typical age-related changes: Losing things from time to time
|
According to the Alzheimer’s Association, typically at least two core mental functions on the following list must be impaired to be considered dementia:
- Memory
- Communication and language
- Ability to focus and pay attention
- Reasoning and judgment
- Visual perception
If You Have Memory Problems, Switch to a Ketogenic Diet
If your memory slips often enough to put even an inkling of concern or doubt in your mind, or if you’ve noticed some unusual mood or behavioral changes, it’s time to take action.
A high-fat, moderate-protein and low-net-carb ketogenic diet is crucial for protecting your brain health and is recommended for virtually everyone, but especially for those who have concerns about their brain health. This type of diet involves restricting all but non-starchy vegetable carbs and replacing them with low to moderate amounts of high-quality protein and high amounts of beneficial fat.
It’s a diet that will help optimize your weight and reduce your risk of chronic degenerative disease while protecting your brain. Eating this way will help you convert from carb-burning mode to fat-burning mode, which in turn triggers your body to produce ketones (also known as ketone bodies or ketoacids).
Ketones can feed your brain and prevent brain atrophy. They may even restore and renew neuron and nerve function in your brain after damage has set in. In addition to eating a ketogenic diet, a primary source of ketones is the medium-chain triglycerides (MCTs) found in coconut oil. As noted in the British Journal of Nutrition:16
“Unlike most other dietary fats that are high in long-chain fatty acids, coconut oil comprises medium-chain fatty acids (MCFA). MCFA are unique in that they are easily absorbed and metabolised [sic] by the liver, and can be converted to ketones. Ketone bodies are an important alternative energy source in the brain, and may be beneficial to people developing or already with memory impairment, as in Alzheimer’s disease (AD).”
Dietary Strategies to Help Prevent Alzheimer’s
Alzheimer’s disease has grown to be one of the most pressing and tragic public health issues facing the U.S. Since there is currently no cure for this disease, prevention remains the best strategy to fight it. The beauty of following my nutrition plan is that it helps prevent and treat virtually all chronic degenerative diseases, including dementia. The sooner you begin, the better. In addition to following a ketogenic diet, the following dietary strategies are also important:
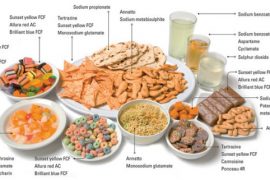
| ✓ Avoid sugar and refined fructose. Ideally, you’ll want to keep your sugar levels to a minimum and your total fructose below 25 grams per day, or as low as 15 grams per day if you have insulin/leptin resistance or any related disorders. |
| ✓ Avoid gluten and casein (primarily wheat and pasteurized dairy, but not dairy fat, such as butter). Gluten also makes your gut more permeable, which allows proteins to get into your bloodstream where they don’t belong. That then sensitizes your immune system and promotes inflammation and autoimmunity, both of which play a role in the development of Alzheimer’s. |
| ✓ Optimize your gut flora by regularly eating fermented foods or taking a high-potency and high-quality probiotic supplement. |
| ✓ Increase consumption of healthy fats, including animal-based omega-3. Sources of healthy fat include avocados, butter made from raw grass-fed organic milk, organic pastured egg yolks, coconuts and coconut oil, raw nuts, raw dairy, grass-fed meats and pasture-raised poultry. Also, make sure you’re getting enough animal-based omega-3 fats.
High intake of the omega-3 fats EPA and DHA help by preventing cell damage caused by Alzheimer’s disease, thereby slowing down its progression, and lowering your risk of developing the disorder. |
| ✓ Reduce your overall calorie consumption and/or intermittently fast. Ketones are mobilized when you replace carbs with coconut oil and other sources of healthy fats. Intermittent fasting is a powerful tool to jumpstart your body into remembering how to burn fat and repair the inulin/leptin resistance that is a primary contributing factor for Alzheimer’s. |
| ✓ Improve your magnesium levels. There is some exciting preliminary research strongly suggesting a decrease in Alzheimer’s symptoms with increased levels of magnesium in the brain.
Unfortunately, most magnesium supplements do not pass the blood-brain barrier, but magnesium threonate appears to and holds some promise for the future for treating this condition and may be superior to other forms. |
| ✓ Eat a nutritious diet rich in folate. Vegetables, without question, are your best form of folate, and we should all eat plenty of fresh raw veggies every day. Avoid supplements like folic acid, which is the inferior synthetic version of folate. |
General Lifestyle Guidelines for Alzheimer’s Prevention
Besides diet, there are a number of other lifestyle factors that can contribute to or hinder neurological health. The following strategies are therefore also important for any dementia prevention plan:
| ✓ Exercise. Exercise leads to hippocampus growth and memory improvement,17 and it’s been suggested that exercise can trigger a change in the way the amyloid precursor protein is metabolized, thus slowing down the onset and progression of Alzheimer’s.18
Exercise also increases levels of the protein PGC-1alpha. Research has shown that people with Alzheimer’s have less PGC-1alpha in their brains and cells that contain more of the protein produce less of the toxic amyloid protein associated with Alzheimer’s.19 |
| ✓ Optimize your vitamin D levels with safe sun exposure. Strong links between low levels of vitamin D in Alzheimer’s patients and poor outcomes on cognitive tests have been revealed.
Researchers believe that optimal vitamin D levels may enhance the amounts of important chemicals in your brain and protect brain cells by increasing the effectiveness of the glial cells in nursing damaged neurons back to health. Vitamin D may also exert some of its beneficial effects on Alzheimer’s through its anti-inflammatory and immune-boosting properties. Sufficient vitamin D (50 to 70 ng/ml) is imperative for proper functioning of your immune system to combat inflammation that is also associated with Alzheimer’s. |
| ✓ Avoid and eliminate mercury from your body. Dental amalgam fillings, which are 50 percent mercury by weight, are one of the major sources of heavy metal toxicity. However, you should be healthy prior to having them removed.
Once you have adjusted to following the diet described in my nutrition plan, you can follow the mercury detox protocol and then find a biological dentist to have your amalgams removed. |
| ✓ Avoid and eliminate aluminum from your body. Sources of aluminum include antiperspirants, non-stick cookware and vaccine adjuvants. For tips on how to detox aluminum, please see my article “First Case Study to Show Direct Link between Alzheimer’s and Aluminum Toxicity.” |
| ✓ Avoid flu vaccinations as many contain both mercury and aluminum, well-known neurotoxic and immunotoxic agents. |
| ✓ Avoid anticholinergics and statin drugs. Drugs that block acetylcholine, a nervous system neurotransmitter, have been shown to increase your risk of dementia. These drugs include certain nighttime pain relievers, antihistamines, sleep aids, certain antidepressants, medications to control incontinence and certain narcotic pain relievers.
Statin drugs are particularly problematic because they suppress the synthesis of cholesterol, deplete your brain of coenzyme Q10 and neurotransmitter precursors and prevent adequate delivery of essential fatty acids and fat-soluble antioxidants to your brain by inhibiting the production of the indispensable carrier biomolecule known as low-density lipoprotein. |
| ✓ Challenge your mind daily. Mental stimulation, especially learning something new, such as learning to play an instrument or a new language, is associated with a decreased risk of Alzheimer’s. Researchers suspect that mental challenge helps to build up your brain, making it less susceptible to the lesions associated with Alzheimer’s disease. |
Sources and References
- 1 World Health Organization March 2015
- 2, 3 Alzheimer’s Association, What Is Dementia?
- 4, 5, 7 The New York Times July 26, 2016
- 6 Fox News February 1, 2017
- 8 Alzheimer’s Association, 10 Signs and Symptoms of Alzheimer’s
- 9 Neurology January 14, 2015
- 10 Time January 14, 2015
- 11 Alzheimer’s Association July 24, 2016
- 12 Alzheimer’s Association, Mild Cognitive Impairment
- 13 Mirror November 9, 2016
- 14 Independent February 2016
- 15 Alzheimer’s Association, 10 Signs of Alzheimer’s
- 16 Br J Nutr. 2015 Jul 14;114(1):1-14.
- 17 Journal of Alzheimer’s Disease, 2011: 25(1); 151-62
- 18, 19 Journal of Neuroscience, April 27, 2005: 25(17); 4217-4221